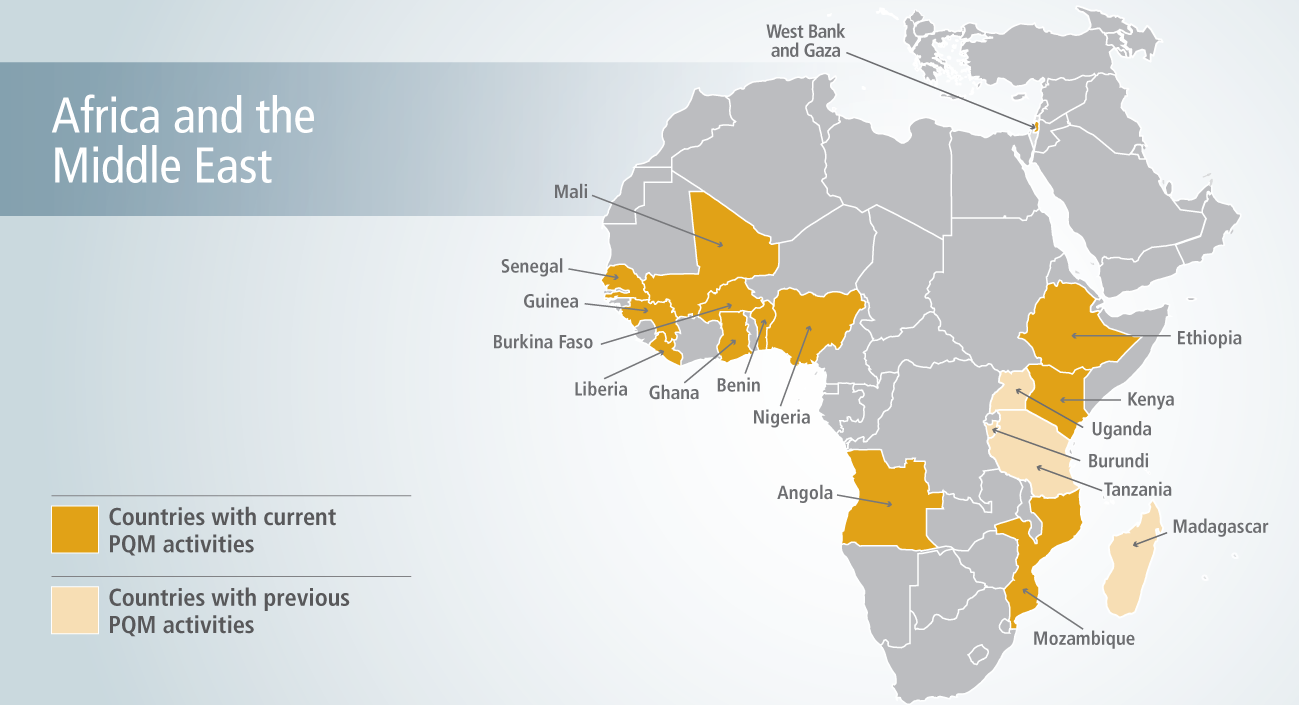
Promoting the Quality of Medicines (PQM) provides technical assistance to strengthen pharmaceutical quality assurance systems in Africa and the Middle East. We have local field-based operations in Ethiopia and Nigeria, and currently support activities in 13 countries in the region.
Our Work in the Region
Strengthen National Regulatory Systems
- Four African countries—Ethiopia, Ghana, Nigeria, and Kenya—have received ISO 17025 accreditation with PQM’s support. Achieving ISO accreditation status demonstrates the laboratories’ technical competence to produce precise and accurate data according to international quality standards. In FY 2016, the national quality control labs in Ghana, Kenya, and Nigeria successfully maintained ISO accreditation. In Nigeria, this resulted in an agreement with the Global Fund and Society for Family Health to test medicine samples at the lab, which will generate income to support sustainability. The accreditation has also allowed the lab to reduce its backlog from over 1,000 samples in 2015 to 200, by no longer needing to send samples abroad.
- In West Bank/Gaza, with PQM’s assistance, the lab is now able to conduct interlaboratory testing, which enhances its prospects for accreditation.
- In Ethiopia, the Product Quality Assessment Directorate’s laboratory received ISO 4074 accreditation, making it the first government laboratory in East Africa to receive an ISO accreditation for medical devices (condom testing). In 2016, the lab’s tests found 39 of 60 condom batches to be substandard; as a result, 141 batches (worth approximately $2 million) were banned from distribution, attesting to the lab’s increased capacity to safeguard public health.
- In Nigeria, the National Council on Health adopted the country’s first documented Quality Assurance Policy. The policy was developed by the Federal Ministry of Health with PQM’s support. It mandates quality assurance and quality control considerations throughout Nigeria’s pharmaceutical supply chain, helping to secure it from falsified and substandard medicines, ultimately protecting patients.
- PQM supported the establishment of a national quality control lab in Liberia where pharmaceuticals are tested, providing evidence for government enforcement actions, including removal of counterfeit medicines from the national market. Twenty counterfeiters were prosecuted; their illicit outlets closed; and all confiscated medicines destroyed. Building a robust post-marketing surveillance program and a strong registration system has enabled Liberia’s regulatory authority to impose continuous and decisive regulatory measures to protect the public from exposure to poor-quality medicines.
- In Ethiopia, PQM advocated for inclusion of antiretroviral, antimalarial, reproductive health, and anti-tuberculosis medicines and vaccines into a fast-tracked registration system. This reduced the average time to register new applications for high-priority medicines from 25 to 17 months. Patients can now access quality-assured lifesaving medicines 8 months sooner than they could before.
Increase Availability of Quality-Assured Medicines
- PQM supports manufacturers of essential medicines in Nigeria and Ethiopia to become compliant with internationally accepted standards. In collaboration with the Chlorhexidine Working Group, chaired by PATH, PQM helped manufacturers bring to scale WHO-recommended 7.1% chlorhexidine digluconate for umbilical cord care of newborns in areas with high neonatal mortality. PQM provided technical assistance to Drugfield Pharmaceuticals in Nigeria to help build their capacity to produce chlorohexidine gluconate according to international quality standards. PQM also developed a monograph for regulators and manufacturers to use to test the quality of these medicines. In Ethiopia, 60 inspections for Good Manufacturing Practices were conducted with PQM support in FY16, a significant increase from FY15 when none were conducted. This further ensures that medicines are manufactured according to established and recognized standards.
Increase Capacity to Detect Falsified, Substandard, and Unapproved Medical Products
- PQM-supported post-marketing surveillance programs in nine African countries are currently collecting data and evidence that enables governments to take regulatory actions on medicines that do not conform to set quality standards. These programs led to regulatory actions against poor-quality medicines in Ghana, Nigeria, Benin, and Liberia this past year, protecting patients from sub-optimal treatment.
- In Nigeria, PQM provided support for medicines quality monitoring sampling in six zones. Data from the surveys showed the presence of poor-quality antimalarial and medicines for maternal, newborn, and child health. Nigerian officials put a hold on further distribution of the affected drugs, led a medicine mop-up exercise at various locations, and will begin possible prosecution.
- Post-marketing surveillance of uterotonic drugs (medicines used in childbirth) was conducted in 10 regions in Ghana. It revealed 57–73 percent of medicines tested were substandard; two counterfeit medicines were also reported. Ghana’s FDA took swift regulatory action based on these data.
- Improved registration of medicines in several African countries has led to immediate recognition of unregistered medicines during monitoring and surveillance activities at sentinel sites and ports where shipments of medicines are frequently received.
Increase Evidence-Based Decision Making
- Communications campaigns about the dangers of falsified and poor-quality medicines in Senegal resulted in expulsion of all medicine sellers at Keur Serigne Be, a major illicit market.
