Collaboration aims to build capacity for inspection of contract research organizations and assessment of bioequivalence studies in East Africa
July 5, 2017
USP and World Health Organization (WHO) collaborated to offer a new training to enhance regional capacity for implementing current International Conference on Harmonisation (ICH) and World Health Organization (WHO) good clinical practice (GCP) guidelines. The workshop took place from June 26-30 in Addis Ababa, Ethiopia and was attended by representatives from the East African Community’s Medicines Regulatory Harmonization (EAC MRH) Programme - regulators who are involved in the inspection of contract research organizations (CROs) and the assessment of bioequivalence (BE) data for marketing authorization. Utilization by the attendees of the information taught during the training will enhance regional capacity for implementing GCP regulations and inspection of CROs conducting clinical trials, in support of the African Medicines regulatory Harmonisation (AMRH) initiative.

A WHO-prequalification team member performs a mock inspection at the RBEC clinical trial bed facility as part of the workshop training.
Participants included more than 10 regulatory professionals from four EAC member states, including Burundi, Rwanda, the United Republic of Tanzania, and Uganda; two inspectors from Ethiopia’s Food, Medicine and Health Care Administration and Control Authority; and three staff members from RBEC. Two representatives from the EAC-MRH secretariat were also in attendance. According to John Patrick Mwesigye, EAC-MRH Health, “The training on GCP regulation and CRO inspection has come at the right time when the EAC partner states are at the nick of implementation of the medicines regulatory harmonized technical guidelines and requirements. It has brought to light the need for the EAC region to make BE requirements a priority as we look forward to ensure and guarantee the efficacy, safety and quality of generic pharmaceutical products available to our patients.”
The workshop was facilitated by Promoting the Quality of Medicines (PQM), a program funded by USAID and implemented by USP, and WHO prequalification and regulatory system strengthening teams. They focused on many aspects of the current ICH and WHO GCP guidelines, including the: design, approval, recruitment, conduct, analysis, monitoring, inspection, and reporting of clinical trials, while emphasizing the application of GCPs to BE studies. The training consisted of classroom lectures, case studies, and a mock inspection of the Regional Bioequivalence Center (RBEC) in Addis Ababa, which allowed participants to gain hands-on experience with the concepts presented in the classroom.
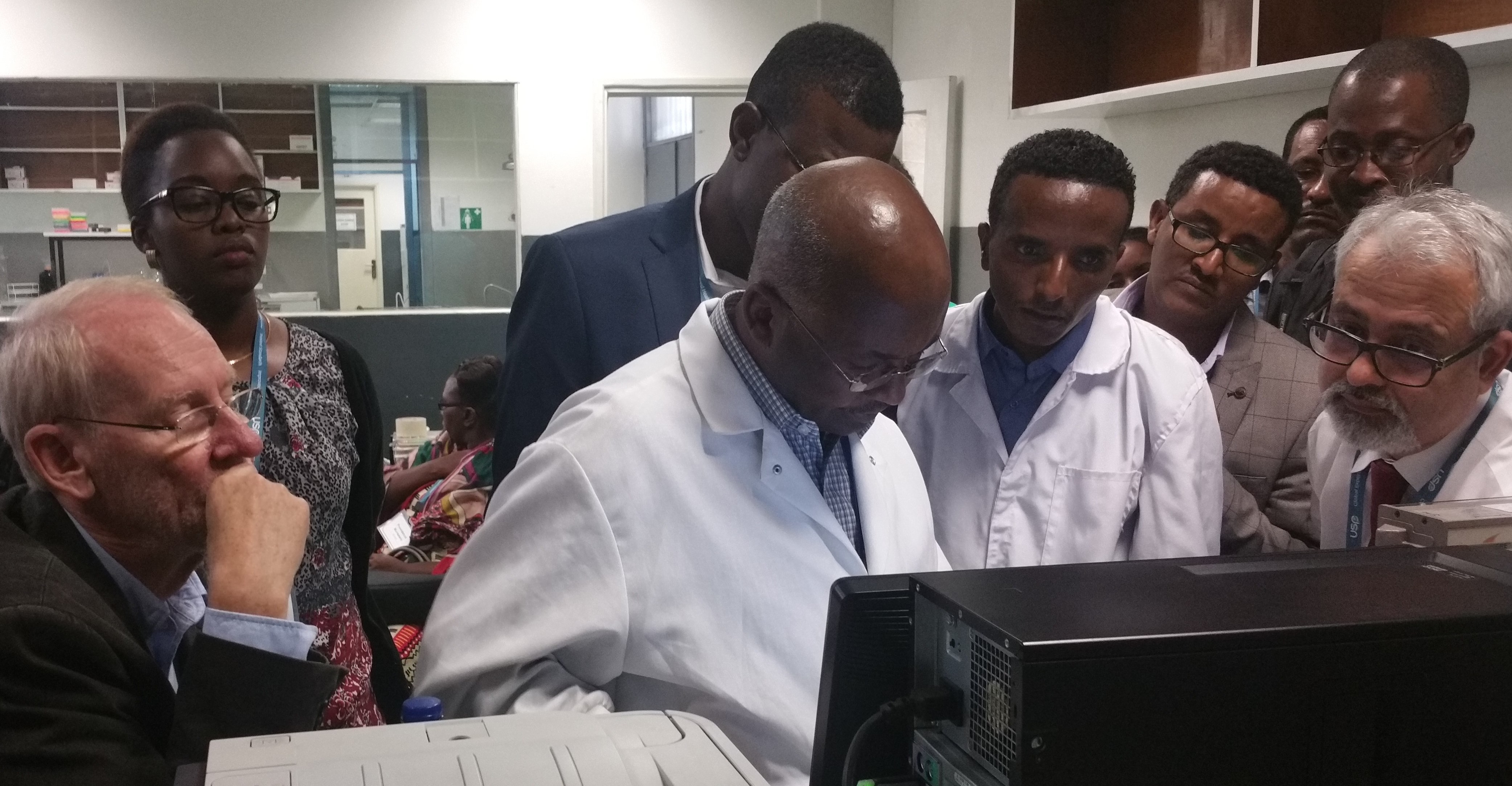
Workshop participants observe RBEC staff discussing chromatographic data during the mock inspection of the RBEC bioanalytical laboratory.
While strengthening the capacity of medicines regulatory authorities (MRAs), the workshop also built on PQM’s ongoing technical assistance to RBEC, which is preparing to host a WHO inspection. If successful, RBEC will be the only WHO prequalified BE center in East Africa. Having a CRO capable of performing bioequivalence studies in compliance with GCP standards means that regulators will be able to confirm the safety and efficacy of generic medicines supplied to patients in the region.
During his presentation, Dr. Paul Nkansah the Deputy Director of PQM noted that, “in building the capacity for GCPs in clinical trials such as bioequivalence studies, we are seeking to ensure that regulators will soon be able to confirm that generic medicines supplied to patients in the region are identical in safety and efficacy to the innovator product.”
In describing her takeaways from the training, Dr. Rachel Kyeyune Bakyayita, Drug Information Officer in Clinical Trials from the National Drug Authority of Uganda, said that “[t]he regulation of clinical trials, especially in resource-limited settings, is challenging, particularly because the line between research and clinical trial BE studies is often gray. This training has equipped me with relevant knowledge and skills in GCP regulations that I can apply to my work.”

Participants gathered outside the RBEC clinical trial study center in Addis Ababa, Ethiopia.
